Imara Inc., a clinical-stage biopharmaceutical company dedicated to developing and commercializing novel therapeutics to treat patients suffering from rare inherited genetic disorders of hemoglobin, today announced that the European Commission granted Orphan Drug designation to IMR-687 for the treatment of patients with sickle cell disease (SCD). IMR-687 has previously been granted Orphan Drug, Fast Track and Rare Pediatric Disease designations from the U.S. Food and Drug Administration (FDA) for the treatment of patients with SCD.
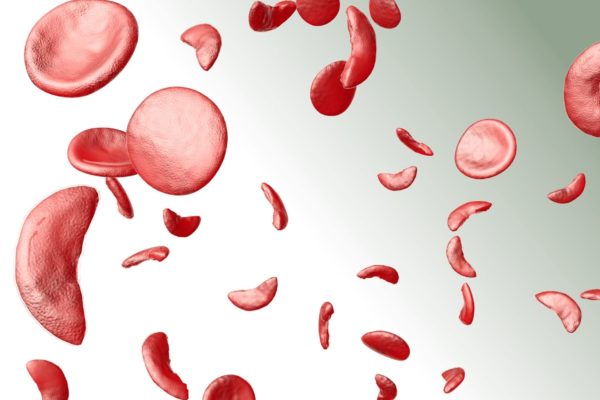
The European decision can lead the way to more effective treatment options for patients with sickle cell disease, a rare blood disorder characterized by debilitating pain, progressive multi-organ damage and early death.
To qualify for Orphan Drug designation in the EU, an investigational medicine must be intended to treat a seriously debilitating or life-threatening condition that affects fewer than five in 10,000 people in the EU, and there must be sufficient non-clinical or clinical data to suggest the investigational medicine may produce clinically relevant outcomes. Orphan Drug designation in the EU provides companies with certain benefits and incentives, including clinical protocol assistance, differentiated evaluation procedures for Health Technology Assessments in certain countries, access to a centralized marketing authorization procedure valid in all EU member states, reduced regulatory fees and ten years of market exclusivity.
IMR-687 is a highly selective and potent small molecule inhibitor of PDE9. PDE9 uniquely degrades cyclic guanosine monophosphate (cGMP), an active signalling molecule that plays a role in vascular biology. Lower levels of cGMP are often found in people with sickle cell disease and beta-thalassemia and are associated with impaired blood flow, increased inflammation, greater cell adhesion and reduced nitric oxide mediated vasodilation.
Blocking PDE9 acts to increase cGMP levels, which are associated with reactivation of foetal hemoglobin, or HbF, a natural hemoglobin produced during foetal development. Increased levels of HbF in red blood cells have been demonstrated to improve symptomology and lower disease burden in patients with sickle cell disease and patients with beta-thalassemia.
Further reading
Read the full press release by Imara on their website.