Zanubrutinib (marketed by BeiGene under the brand name Brukinsa) extends progression-free survival (PFS) in patients with relapsed or refractory chronic lymphocytic leukaemia and small lymphocytic lymphoma (CLL/SLL).
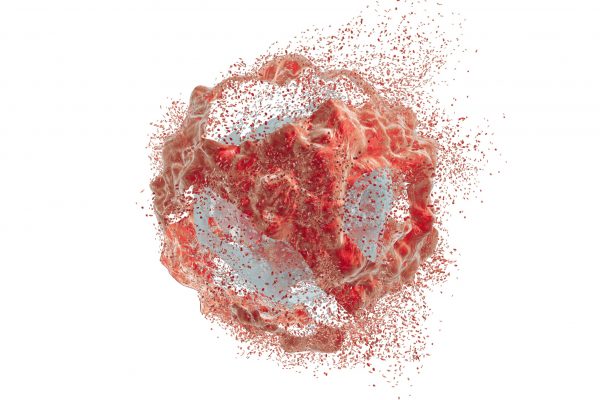
Bruton’s tyrosine kinase (BTK) inhibitors effectively treat CLL and SLL. The ALPINE study has evaluated the efficacy of BTK’s selective inhibitor, zanubrutinib, versus ibrutinib.
Between November 2018 to December 2020, the open-label ALPINE study recruited 652 patients with relapsed or refractory CLL or SLL who had received at least one prior line of therapy. 45% of these patients had bulky disease, with 23% having 17p deletion, TP53 mutation or both. Most patients were white (81%) with a median age of 67 years. The participants were randomised (1:1) to receive either zanubrutinib or ibrutinib.
After a median follow-up of 29.6 months, disease progression was seen in fewer patients (87) after zanubrutinib treatment as compared to the ibrutinib arm (118, HR 0.65, 95% CI 0.49-0.86, P=0.002). Further, the progression-free survival (PFS) was higher with zanubrutinib vs ibrutinib (78.4% vs 65.9%). A similar situation was observed in the highest-risk group of 17p deletion, a TP53 mutation, or both with zanubrutinib (24 and 36 occurrences of disease progression or death; HR 0.53, 95% CI 0.31-0.88).
The overall response rate was also higher in the zanubrutinib arm compared to the ibrutinib treatment (86.2% vs 75.7%).
Fewer treatment-related adverse events (AEs) with zanubrutinib (42% vs 50%), dose interruptions (50% vs 56.8%), and discontinuation of treatment (15.4% vs 22.2%) were observed.
The findings of the ALPINE study show the efficacy of oral BTK inhibitor zanubrutinib for patients with refractory or relapsed CLL/SLL.