Luspatercept is a recombinant fusion protein that binds transforming growth factor β superfamily ligands to reduce SMAD2 and SMAD3 signaling. Two international phase 3 studies were recently published in the New England Journal of Medicine, in which the effectiveness of luspatercept was examined in relation to reducing dependency on red-cell transfusions. The MEDALIST clinical trial focused on the use of luspatercept in very-low-risk, low-risk, or intermediate-risk MDS patients with ring sideroblasts. The BELIEVE clinical trial examined the effect of luspatercept in patients with transfusion-dependent β-thalassemia.
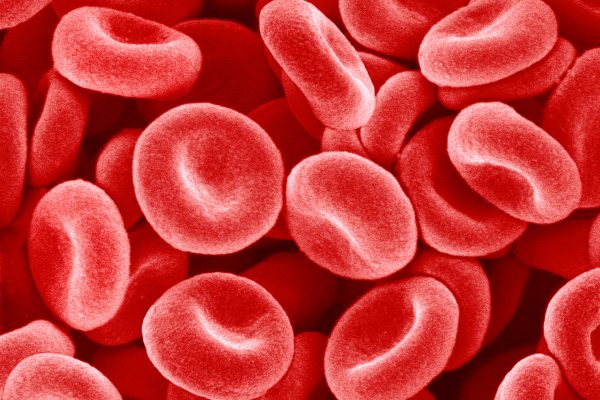
β-thalassemia is a hereditary hemoglobinopathy that is characterized by ineffective erythropoeiesis and impaired maturation of red blood cells. The disease is associated with potentially life threatening conditions such as severe anemia and organ damage. The BELIEVE trial was a randomised double blind phase 3 trial in which 336 adult β-thalassemia patients were treated for a median of 64 weeks with best supportive care, combined with either luspatercept or placebo in a 2:1 ratio.
The primary end point was the percentage of patients who had a reduction in the transfusion burden of at least 33% from baseline during weeks 13 through 24 plus a reduction of at least 2 red-cell units over this 12-week interval. Other efficacy end points included reductions in the transfusion burden during any 12-week interval and results of iron studies.
The percentage of patients who had a reduction in the transfusion burden of at least 33% from baseline during weeks 13 through 24 plus a reduction of at least 2 red-cell units over this 12-week interval was significantly greater in the luspatercept group than in the placebo group (21.4% vs. 4.5%, P<0.001). During any 12-week interval, the percentage of patients who had a reduction in transfusion burden of at least 33% was greater in the luspatercept group than in the placebo group (70.5% vs. 29.5%), as was the percentage of those who had a reduction of at least 50% (40.2% vs. 6.3%). Adverse events such as bone pain, dizziness, hypertension, and hyperuricemia were more common with luspatercept than placebo.
The MEDALIST trial included 229 patients with very-low-risk, low-risk, or intermediate-risk myelodysplastic syndrome (MDS) with ring sideroblasts who had been receiving regular red-cell transfusions. Of these 229 patients, 153 received luspatercept (at a dose of 1.0 up to 1.75 mg per kilogram of body weight) and 76 received placebo, administered subcutaneously every 3 weeks. The primary end point was transfusion independence for 8 weeks or longer during weeks 1 through 24, and the key secondary end point was transfusion independence for 12 weeks or longer, assessed during both weeks 1 through 24 and weeks 1 through 48.
Transfusion independence for 8 weeks or longer was observed in 38% of the patients in the luspatercept group, as compared with 13% of those in the placebo group (P<0.001). A higher percentage of patients in the luspatercept group than in the placebo group met the key secondary end point (28% vs. 8% for weeks 1 through 24, and 33% vs. 12% for weeks 1 through 48; P<0.001 for both comparisons). The most common luspatercept-associated adverse events included fatigue, diarrhea, nausea, and dizziness. The incidence of adverse events decreased over time.
Both trials show that luspatercept can effectively reduce the severity of anemia associated with β-thalassemia and MDS, and few adverse events led to the discontinuation of treatment. Luspatercept is the first medicine of its kind. Luspatercept has been approved by the EMA for use in the mentioned conditions. Luspatercept is produced by Celgene.
MEDALIST-trial: Fenaux P, Platzbecker U, Mufti GJ, et al. Luspatercept in patients with lower-risk myelodysplastic syndromes. N Engl J Med 2020;382:140-51.
The UZ-A hospital in Antwerp provides information in Flemish on β-thalassemia on its website.
Website Gezondheid.be also contains comprehensive information.
For French speakers there is also the website of the Association Belge de Thalassemie.